In this post
Lorem ipsum dolor sit amet
Lorem ipsum dolor sit amet
Fourteen million U.S. adults owe $1000+, and 3 million owe more than $10,000 in medical debt, according to the Kaiser Family Foundation. Put it all together, and that’s $220 billion in collective medical debt in 2024—enough to fund NASA’s budget for nearly a decade.
With medical expenses expected to increase by 8.9% this year, employers must be savvy about how they support their workers with health insurance. A health reimbursement arrangement (HRA) is one way they can do this.
What is a health reimbursement arrangement?
A health reimbursement arrangement is an employer-funded plan that reimburses employees for any out-of-pocket medical expenses they clock up. The reimbursement can cover a wide range of medical costs, including deductibles, prescription drugs, and medical equipment. Some employers offer HRAs to supplement their health coverage, but others provide them instead of group health insurance.
HRAs offer tax advantages for both employers and employees. Employers claim a tax deduction for the reimbursements they provide, while employees’ reimbursements are typically tax-free.
How does a health reimbursement arrangement work?
The following steps are involved in setting up and using an HRA:
- The employer decides how much money to put into the HRA to cover medical expenses for each worker. Employers must provide the same HRA contribution for each employee in the same class.
- Employers decide which expenses to make eligible for reimbursement.
- If employees incur eligible medical expenses, they can request reimbursement up to the set value of their HRA. Employees must first incur the expense before requesting reimbursement; however, some benefits providers provide an HRA debit card to offer immediate reimbursement at the point of payment.
Who can offer an HRA?
HRAs are a go-to benefits choice for employers of any size or type. However, the type of HRA they offer depends on factors like the size of the company and any existing health insurance coverage. Some types of HRAs include:
Qualified small employer HRA (QSEHRA)
Qualified small employer HRAs are available to employers with less than 50 full-time employees. They’re ideal for small businesses that want to provide health benefits but aren’t able or willing to invest in a traditional group health insurance plan.
The Internal Revenue Service’s “Employer’s Guide to Fringe Benefits” sets the employers’ contribution limit for HRAs at $6,150 per individual and $12,450 per family in 2024.
Individual coverage HRA (ICHRA)
Individual coverage HRAs have been available since January 2020, before which it wasn’t possible to use HRAs to fund individual health insurance premiums. ICHRAs don’t have minimum or maximum contribution limits. Employers can simply choose how much they want to contribute to their employees’ ICHRAs, providing greater flexibility when designing benefits packages.
Integrated or group coverage HRA
Integrated HRAs work well in conjunction with another group health plan. These HRAs allow employers to provide an additional source of funding for employees to pay for out-of-pocket medical expenses not covered by the primary group health plan. For example, if an employee’s spouse is covered under a different employer’s group health plan, an Integrated HRA can plug any gaps in the coverage and make healthcare more affordable for the couple.
Excepted Benefit HRAs
Excepted benefit HRAs (EBHRAs) were introduced in January 2020. They cover limited benefits, such as dental and vision expenses, not covered by a primary group plan. EBHRAs have a maximum contribution limit of $2,100 for 2024. Unlike integrated HRAs, employees do not need to participate in their employer’s group plan to use an EBHRA and receive reimbursements.
HRA vs. HSA vs. FSA
Confused by the different acronyms tossed around in the benefits world? Here’s how to distinguish between HRA vs. HSA and FSA.
- Health reimbursement arrangements (HRAs) are entirely employer-funded. Employees are reimbursed for their HRA eligible expenses, and any unused funds are returned to the employer or may be rolled over to the following year, depending on the plan’s specific terms.
- Health savings accounts (HSAs) are available to employees enrolled in high-deductible health plans (HDHPs). They’re funded by both employers and employees, who can contribute pre-tax dollars to their HSA account. Withdrawals are tax-free when used for qualified medical expenses.
- Flexible spending accounts (FSAs) are also funded by employers and employees using pre-tax dollars to pay for eligible healthcare expenses. Employees must use their funds within the plan year, although a limited carryover option may be available.
What are the benefits of offering HRAs?
So, why opt for an HRA above other types of healthcare benefits? While each employee and employer must consider the right option for their specific situation, HRAs offer some broad advantages, as follows:
1. They’re inclusive and accessible for all employees.
Versatility tops the HRA pro list. Employers can set up their healthcare reimbursement arrangements with different contribution levels to cover various medical expenses, from routine doctor visits and prescriptions to more specialist care, such as mental health services.
With different HRAs available, employers select the option that best matches their company’s size and structure and their employees’ healthcare requirements.
2. They offer tax advantages for employers and employees.
HRAs offer tax advantages for everyone involved. Employees can reduce their overall taxable income, while employees’ reimbursements for qualifying medical expenses are exempt from federal income taxes.
3. They’re compatible with other health benefits packages.
HRAs combine well with other healthcare plans in your benefits stack to ensure 360-degree wellness for your employees. This holistic approach allows employees to tailor their healthcare coverage according to their individual needs and situations, potentially filling any gaps that a single health benefits package might leave uncovered.
The bottom line: HRAs are an inclusive and accessible benefit for all employees, providing meaningful support for their healthcare needs.
HRA administration best practices
Ready to roll up your sleeves and start offering HRAs for your people? Consider the following best practices:
Understand your compliance requirements
Know the ins and outs of HRA compliance before you enroll employees in your benefits plans. There are specific rules and regulations to follow, such as:
- IRS regulations: The IRS outlines requirements for eligibility, allowable expenses, and contribution limits. Benefits administrators must also keep proper documentation and report HRA contributions and reimbursements.
- Affordable Care Act (ACA): The ACA mandates that all health plans, including HRAs, must meet certain standards. The guidance ensures that HRAs can be integrated with ACA-compliant group health plans and offered in a way that meets these requirements.
- Non-discrimination tests: HRAs must be available on equal terms to all eligible employees to prevent discrimination based on health status or employment classification.
- Health Insurance Portability and Accountability Act (HIPAA): This governs how employees’ personal health information is handled.
Employers considering offering an HRA must carefully review these compliance requirements to ensure their plans are effective for employees and legally sound.
Invest in benefits software
Give yourself a helping hand in meeting HRAs’ many compliance requirements by leaning on dependable software. The right platform will:
- Ensure compliance with all regulatory requirements, including new updates
- Simplify HRA administration processes for your People and Finance teams
- Minimize any manual errors to save money and keep your employees happy
- Promise extra privacy for your employees’ sensitive medical information
Always do your homework before you select a particular HRA vendor. Read software platform reviews, consult customer case studies, and make use of customer demos and software trials to explore how specific software features will enhance your processes.
Automate your system
The right benefits platform will include automation capabilities, enabling you to simplify repetitive processes that would otherwise be prone to error and may eat into your time. Automation offers the following features:
- Delivering automatic HRA reimbursements
- Verifying expenses to ensure they’re eligible
- Generating plan documents to meet your compliance requirements and provide excellent employee communications
Offer personalized healthcare with Benepass
Benepass HRA is the perfect solution for any organization with a diverse employee base. Using our streamlined platform, you’ll offer tax-free funds to pay for various eligible medical expenses, such as:
- Fertility treatments
- Gender confirmation surgery
- Healthcare-related travel
- Mental health services
Here’s how it works:
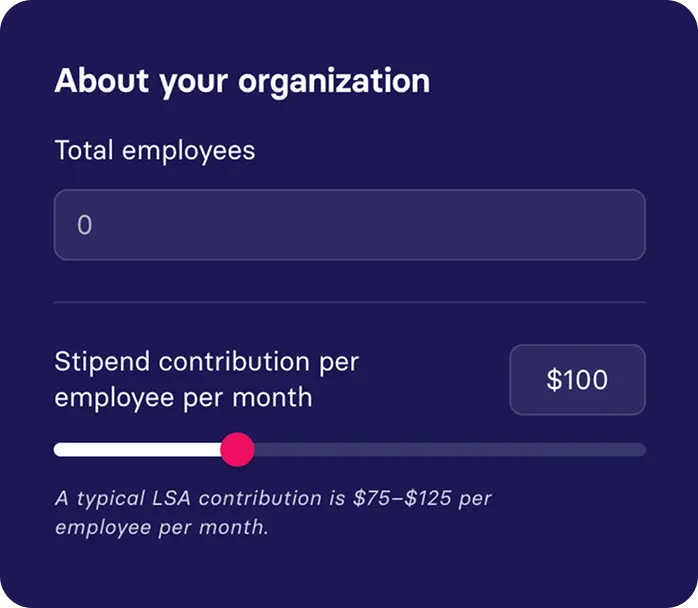
- Employers define how their program works by choosing their eligible expense categories.
- Employers determine how much they want to contribute to their employees’ HRAs.
- Benepass connects to your payroll system and automatically enrolls eligible employees.
- Employees can start using their HRA.
Ready to empower your employees with personalized healthcare? Request a free Benepass demo or connect with a benefits specialist today.



.jpg)